Causes and symptoms of cervical lesions
Anterior Cervical Discectomy and Fusion (ACDF) is a surgical procedure to treat cervical spine lesions. Most cervical lesions are caused by degenerative, strain or accidental injuries. The disease can occur in the cervical intervertebral discs, the facet joints of the cervical spine, or the bones of the cervical spine. The center of the cervical spine is cervical cord that responsible for controlling our limbs, trunk, and bowel movements. Instability of the cervical spine can cause muscle tension, neck and upper back pain, shoulder pain and headaches. Nerve compression will cause sensory nerve and motor nerve dysfunction. Patients will experience numbness and pain of the hand and foot, muscle weakness, gait imbalance, frequent urination and constipation. In addition, the dysfunction of the reflex nerve and the sympathetic vagus nerve can also cause dizziness, tinnitus, gastrointestinal discomfort and even emotional instability.
Case Sharing
Mr. Lu, 55 years old, is an engineer. He came to see the author in November 2016. In the past two years, he has numbness and pain in his hands, especially the thumb and two fingers of his right hand. Later, he has weak hands and weak feet when walking. He visited Western and Chinese medicine in different disciplines for two years, and also received conservative treatment from physiotherapist and chiropractors. The clinical examination showed that Mr. Lu may be severely cervical cord compression. The MRI confirmed that the C4-6 had severe degeneration and intervertebral disc herniation, and severe compression to the spinal cord, the cord is deformed, flat and edema. (See Figure 1)
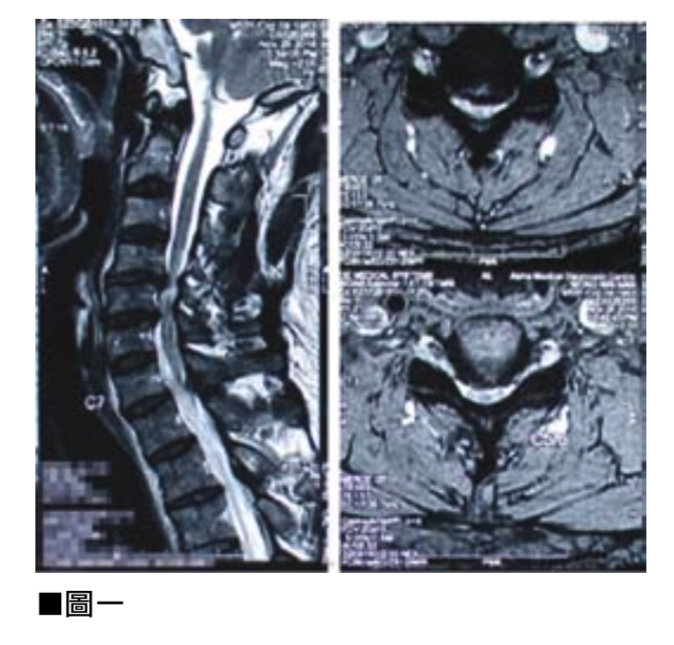
Fig 1 - severe cervical cord compression
Due to the serious condition, the author suggested that Mr. Lu undergo surgical cervical decompression and fusion. However, after consulting his relatives and friends, he was worried about the risk of nerve damage and paralysis of the limbs and lower body, so he refused to perform the operation and chose to continue the conservative treatment. However, Mr. Lu’s condition was deteriorating, it was even difficult to draw a pen with his hands and eat with chopsticks. There were also several accidents where he stumbled and fell and caused head injuries. The problem with his cervical spine is serious, as long as the cervical spine is slightly injured, it will permanently damage the spinal cord and having the risk of permanent paralysis of the limbs. Surgery is a must in order to relief his symptoms.
Finally, Mr. Lu listened to the author’s medical opinion and was admitted to the hospital for four-hour minimally invasive surgery-anterior cervical discectomy and vertebral body fusion. The purpose of the surgery was to decompress the central nerve of the spinal cord and consolidate the stability of the cervical spine. After the operation, Mr. Lu stayed in bed for one night. The next morning he found that his limbs no longer felt numb and painful, and the muscle strength of his limbs had also improved significantly. Under the author’s supervision, he got out of bed and walked around. He found that the feeling when his feet were standing on the ground was much stronger and more stable than before the operation. The strength of both feet improved significantly while walking quite smoothly. According to X-ray and MRI observations, the compression of the cervical spinal cord has been greatly decompressed. (See Figure 2) Mr. Lu was discharged from the hospital and went home 24 hours after the operation that afternoon.
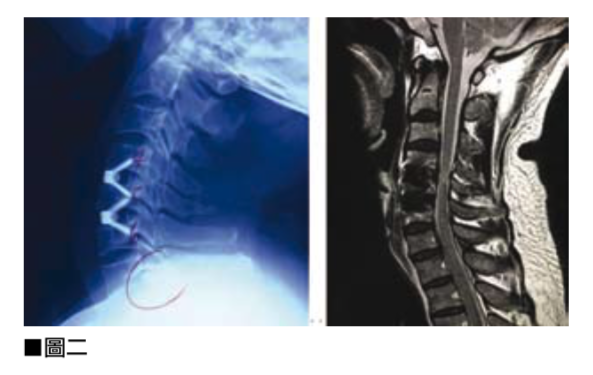
Fig 2 - fusion of cervical spine
What is “anterior cervical discectomy and fusion"?
After general anesthesia, the operation is usually performed for three to four hours via X-ray guidance. Under the microscope, the neurosurgeon will make a small wound of two to three centimeters along the neck lines on the patient’s neck, and then carefully decompress the nerves and remove the discs and bone spurs. On the premise of protecting the nerves, neurosurgeons will use the microscope throughout the entire process, using their skilled fingers and sophisticated neurosurgical instruments to perform operations under the microscope with an amplitude of less than two millimeters and a degree of guideline to ensure the spinal cord. The central nerve and surrounding cervical nerves are fully protected and decompressed. After that, the doctor will implant artificial intervertebral discs to fill the gap between the upper and lower vertebral bodies to stabilize the cervical spine.
Compared with the new type of ACDF surgery, the non-minimally invasive traditional surgery in the past does not use a microscope. Doctors will only use a small piece of the patient’s own pelvic bone to fill the gap between the two cervical vertebrae. The effect of stabilizing the cervical spine and fusion, but the patient has to bear the pain of additional wounds on the pelvis, and before the cervical spine is slowly fused, the patient must also wear a three-month rigid cervical brace to ensure the stability of the cervical spine.
Types and functions of artificial intervertebral discs
As mentioned earlier, artificial intervertebral discs are implanted during surgery. The invention of artificial intervertebral discs is to cooperate with the minimally invasive neurosurgery of the microscope, so as to save the patient’s extra wounds on the pelvis in the traditional operation. In particular, the artificial intervertebral disc can immediately stabilize the patient’s cervical spine, and avoid the inconvenience of wearing a three-month rigid cervical brace. Artificial intervertebral discs can be divided into two types: active or inactive:
Inactive artificial intervertebral disc
It is a combination of synthetic reinforced plastic, artificial bone, and titanium wire. The artificial bone in the artificial intervertebral disc will stimulate the patient’s own bone within six months, and then fuse the upper and lower cervical vertebrae bones together to enhance the stability of the cervical spine. The titanium wire part of the artificial intervertebral disc also immediately stabilizes the cervical spine, so the patient does not need to wear a hard neck brace.
Movable artificial intervertebral disc
It is a combination of synthetic reinforced plastic, reinforced porcelain and titanium metal. Because it is a movable type, the upper and lower cervical vertebrae are not fused, but continue to enjoy flexible activities.
Before the operation, the doctor will discuss with the patient, according to the patient’s condition and needs to determine the number of cervical vertebrae to be operated on, and choose a fixed or non-fixed artificial intervertebral disc. Generally speaking, if the patient’s cervical spine is unstable and causes neck pain or headache, or spinal cord has been severely compressed, the inactive type is the first choice, which can cure the unstable pain and prevent the spinal cord from continuing degenerate in the future. If more than one cervical spine surgery is required, such as involving three cervical vertebrae, the doctor may recommend one or two of them to use movable artificial intervertebral discs, and the rest to use inactive artificial discs. In this way, the stability of the cervical spine can be maintained and a considerable degree can be obtained bringing flexibility to the cervical spine activity. (See Figure 3)

Fig 3 - movable cervical artificial disc
The first task is to protect the central nervous system
In summary, the primary task of a neurosurgeon is to protect the central nervous system, compared to brain surgery, minimally invasive cervical neurosurgery is quite safe and low-risk. The doctor will plan the most appropriate and safe medical plan according to the patient’s condition, in order to cure the patient’s symptoms and help the patient recover to enjoy normal life and activity.

 Book an Appointment
Book an Appointment


