Craniotomy for meningioma brain tumor
Meningioma is the second most common primary intracranial tumor, secondary to glioma, accountable to 15 to 24% of intracranial tumors. It is usually a benign tumor and can be cured completely after surgical removal
The annual incidence of meningioma is about 6 out of every 100,000 people. It can occur at any age, especially in adults between 30 and 50 years old. Most of them are women, and the ratio of male to female is about 1: 2. About 95% of meningiomas are benign. They grow slowly, with an average annual growth rate of 1 to 2 cm or 3.6% of the volume and tend to stay in the patient’s brain for a long time.
It is reported that the average early signs of meningiomas in 2.5 years, and a small number of meningiomas can grow to 6 years. Because the tumor in patients is slow growth rates and is not able to detect earlier, the tumors are usually large by the time the symptoms appear. The neurological symptoms of meningioma’s patients varies on the location of the tumor and the degree of nerve compression. Tumor compression can also cause edema of the brain, increasing intracranial pressure. The most common symptoms are headache, dizziness, numbness or weakness of the hands and feet, unsteady gait, blurred vision, smell or hearing impairment, temperament change, vomiting, epilepsy, nerve pain, etc.
Since meningiomas are benign tumors, they can be cured completely after surgical removal. If it cannot be completely removed, part of the tumor is removed to decompress the nerve, and the result is also good. After partial resection, combined with stereotactic radiotherapy, most meningiomas can be cured. Generally speaking, meningiomas that are larger than the convex surface of the brain are completely removed by neurosurgeons to reduce the chance of recurrence. However, if the location of the tumor is in a dangerous area (such as the inner side of the sphenoid wing, orbit, sagittal sinus, ventricle, pontine cerebellar angle, optic nerve sheath), complete tumor resection may cause permanent damage of nerve function. Therefore, part of the tumor will be removed to only decompress the nerve.
Case Study 1: Benign duramatoma of the skull base with prolapse
In 2015, a 50-year-old female patient from mainland China has symptoms of headache and blurred vision for six months. The magnetic resonance imaging performed in China showed that there’s a 2 cm tumor at the base of the skull extending and compressing the optic nerve, enclosing the aorta (ICA) and anterior brain on both sides (ACA). (See Figure 1)
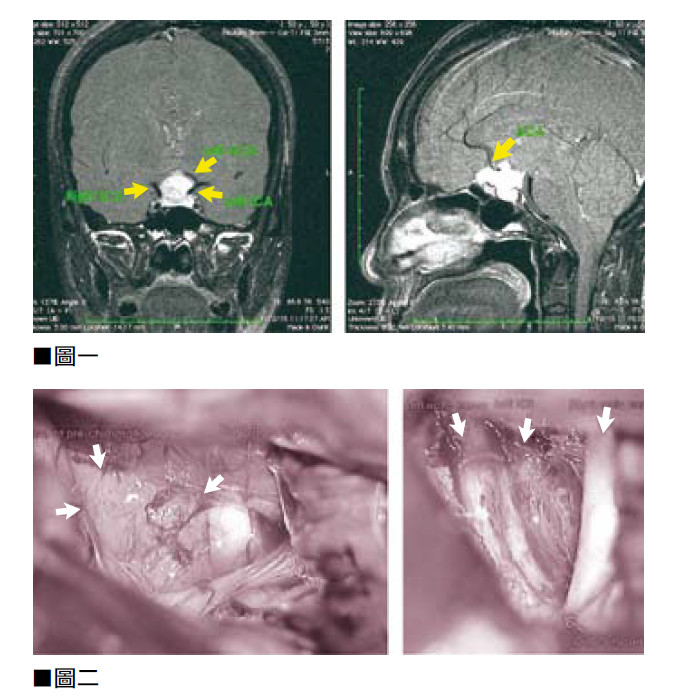
A six-hour minimally invasive craniotomy was performed. The tumor was completely removed under a microscope, and the optic nerve was decompressed. The aorta (ICA) and the anterior cerebral artery (ACA) in both sides of the brain were both intact. (See Figure 2) After the operation, the patient’s vision also returned to normal, and she returned to mainland China three days later. MRI examinations four years later confirmed that the tumor showed no signs of reoccurring.
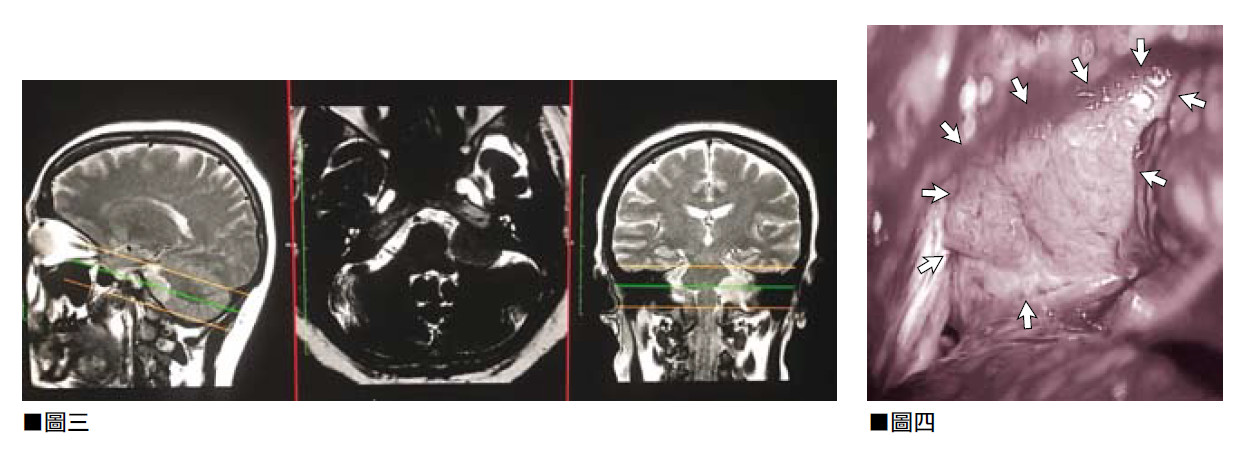
Case Study 2.3 cm benign meningeal tumor on the left petrous slope
Meningioma compresses the CN5 to CN12 nerve in the brain stem and skull base of the patient. (See Figure 3) Symptoms include electric shock-like pain in the left face area. The patient underwent a minimally invasive neurosurgery, under continuous nerve conduction monitoring, the patient underwent a 12-hour minimally invasive microscope neurosurgery to completely remove the tumor. (See Figure 4)
Because the tumor oppresses the nerves of the brainstem and skull base, especially the 7th (facial nerve) and 8th (auditory nerve) nerves of the skull base are severely pushed, causing the nerves to be twisted and deformed. In the process of tumor resection. The author uses a 1 to 2 centimeter surgical tool to operate with precise strength, method and direction and concentrates on finding and protecting nerve from the periphery and inside of the tumor.
Regarding the risks of surgery, the most common nerve damage is permanent loss of hearing, or temporary or permanent facial nerve paralysis. In some cases, the risks and complications of surgery can even cause damage to the brain stem or blood vessels, leading to severe disability or even death. Fortunately, in this surgery, all cranial nerves at the base of the skull, tiny blood vessels, and the main basilar artery of the brainstem and their functions were all well preserved without damage.
In retrospect, this was indeed a very difficult task. After the 12-hour operation, it was already early in the morning, which was twice as long as the 6 hours expected. This was due to the procedures of carefully removing the tumor from the delicate nerves, separating the blood vessels, and separating the tumor from the normal nerve tissue of the brainstem and cerebellum. During the operation, the author’s adrenaline increased with no physical need (eating, drinking, fatigue, and toileting). But after the operation, the shoulders and back were extremely tired and painful, but the end result is very promising.
Due to the complete removal of the tumor, the originally planned postoperative digital navigator electrotherapy is no longer needed. The MRI of the patient one month after the operation and two years after the operation showed that the tumor had been completely removed and there was no sign of recurrence.
most common symptoms are headache, dizziness, numbness or weakness of the hands and feet, unsteady gait, blurred vision, smell or hearing impairment, temperament change, vomiting, epilepsy, nerve pain.

 Book an Appointment
Book an Appointment


