2017-5-12
The Pituitary Gland is located at the center of the bottom of the brain and is the main control center of hormones in the body. What happens if there is a tumor in the pituitary gland?
The normal pituitary gland produces several important hormones, including corticotropin, which stimulates the adrenal glands; thyroid hormones stimulate the thyroid; luteinizing hormone and follicle-stimulating hormone interact with sexual organs; growth hormone helps sugar metabolism and cell growth; lactation hormones affect milk secretion.
Pituitary adenomas are slow-growing among many benign tumors of the pituitary gland, accounting for 10 to 15% of all brain tumors. Those smaller tumors (less than one centimeter in diameter) are called Microadenomas, and larger tumors (greater than one centimeter in diameter) are called Macroadenomas. Pituitary tumors can also be divided into functional and non-functional tumors. According to classification, functional tumors will produce a large amount of irregular hormones. In contrast, non-functional tumors do not produce hormones.
Symptoms of adenoma of the pituitary gland
(1) Overproduction of hormones: The specific symptoms depend on which type of hormone the patient has overproduction. Tumors that produce too much ACTH can lead to Cushing’s disease, which can cause obesity, high blood pressure, muscle weakness and other symptoms; prolactin cell adenoma is a pituitary adenoma that produces a lot of prolactin, and its symptoms include Irregular menstruation, sexual dysfunction, and abnormal breast secretion; growth hormone tumors cause acromegaly, which is an abnormal size of the hands and feet and changes in facial features, such as enlarged cheekbones, prominent brow bones or chin.
(2) Insufficient function of the pituitary gland: non-functional adenomas may also cause hormonal problems. It will oppress the pituitary gland and cause normal hormone decline or stop production.
(3) Lack of visual field: Larger tumors may grow upwards, grow outside the sella and compress the optic nerve. This often leads to a special lack of vision, called bitemporal semiblindness.
(4) Non-specific symptoms: Sometimes a large pituitary adenoma may cause headaches or a feeling of pressure or swelling behind the eyes. Tumor bleeding is more likely to cause severe headaches, double vision, and blurred vision.
The pituitary gland is actually a small gland in the brain. The cause of the tumor is still unknown. Although gene mutations have been found in some patients, this gene mutation does not necessarily cause tumors. In addition, pituitary gland tumors are usually not congenital, are not related to genetics, and may appear at any age.
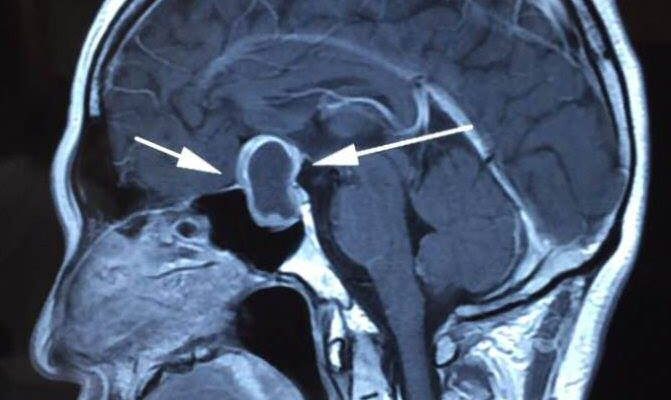
Any patient suspected of having a pituitary adenoma must undergo at least two tests. One is a magnetic resonance scan (MRI) to check the position of the saddle of the brain. This test provides anatomical information to determine whether the adenoma has invaded neighboring structures or appears to be oppressed by the optic chiasm, such as cavernous sinus; the second test is an adequate endocrine blood assessment to determine whether the tumor affects hormone levels. If the tumor is large, a vision assessment and visual field examination are also needed. This test can help diagnose whether the tumor has affected the optic nerve.
Treatment
(1) Medication: Medication is effective for pituitary adenomas that overproduce prolactin and growth hormone. For prolactin cell adenoma, Bromocriptine is quite effective in reducing the blood prolactin level and shrinking the tumor; as for acromegaly caused by the overproduction of growth hormone, it can be treated with Octreotide. Bromocriptine’s effect on tumors that produce growth hormone is generally not effective on prolactinoma.
2) Surgical treatment: The standard treatment for tumors is surgical removal. The goal of surgery is to remove the tumor as safely as possible to reduce the pressure on the optic nerve and to remove tumor cells that overproduce hormones. Most pituitary surgery does not require drilling holes in the scalp and skull. The most common surgical method is the “transsphenoidal method". The operation will go through the sphenoid vein, a space filled with air behind the nose, and under the lips. Or make an incision in the nose, and then remove the tumor in the posterior area of the nose and below the sella turcica. The use of endoscopy through the sphenoid bone to assist in the removal of tumors has become more and more common.
Sometimes microadenoma of the pituitary gland can be found in MRI images, but as long as the condition of the adenoma and the patient’s symptoms are observed regularly, not all patients with pituitary gland tumors needs treatment.
(3) Radiotherapy: If surgery cannot remove the entire tumor, radiotherapy may be a necessary method to control the tumor and prevent its growth. Conventional radiotherapy is to emit a small dose of radiation in the entire area of the sella and the vicinity of the pituitary gland. This technique will also include the marginal normal tissues in the treatment range. Conventional radiation therapy will be completed in a few weeks in a few daily doses. Such therapy is very effective in preventing tumor growth. Although with conventional radiotherapy, the optic chiasm receives as much radiation as the tumor, the risk of visual complications is actually very low.
Radiotherapy surgery CyberKnife (digital navigation knife) is a new option for the treatment of pituitary adenomas. It can focus on the location of the tumor and minimize the amount of radiation absorbed by normal brain tissue. Data show that radiotherapy surgery is more effective than conventional radiotherapy in reducing abnormal hormone production and shortening the treatment time. However, some of the side effects of radiation, such as the risk of vision loss, which is the most fearful for patients, are greatest for patients with brain tumors that are closer to the visual chiasma or hypothalamus. For such high-risk patients, segmented radiotherapy can reduce damage to important brain tissue.

 Book an Appointment
Book an Appointment


