- Home
- Transcranial Magnetic Stimulation (TMS)
Transcranial Magnetic Stimulation (TMS)
Transcranial Magnetic Stimulation (TMS) is a newly launched neurological rehabilitation method for stroke. Magnetic stimulation of the human brain for rehabilitation of stroke has been widely proven to have clinical benefits and effects.
What is magnetic stimulation therapy?
Brain Magnetic Stimulation Therapy (TMS) is non-invasive. It can awaken, restore, replace, and possibly regenerate nerve cell functions by stimulating normal and injured brain cells. After brain magnetic stimulation therapy, the nerve function lost by stroke patients can be recovered more quickly and comprehensively; but in order to achieve the best therapeutic effect, brain magnetic stimulation therapy must be combined with other conventional traditional stroke rehabilitation treatment plans, such as physical therapy, occupational and speech therapy is combined with clinical application. Through the patient’s skull, brain magnetic stimulation therapy stimulates the activity of their brain neurons; the stimulation is caused by short electromagnetic pulses. The intensity of the magnetic field is between 2 and 3 Tesla, similar to a MRI machine. During brain magnetic stimulation therapy, doctors or medical staff will place a hand-held butterfly-shaped coil on the patient’s head to generate precise and highly focused electromagnetic pulses. This is using the concept of electromagnetic induction in physics. Electromagnetic pulses will generate tiny currents in the patient’s brain area to activate brain cells.

During brain magnetic stimulation therapy, doctors or medical staff will place a hand-held butterfly-shaped coil on the patient’s head to generate precise and highly focused electromagnetic pulses.
Brain magnetic stimulation therapy is safe and effective
During the entire treatment process, the patient does not need to inject any anesthetics or sedatives, and always remains awake, but some patients may feel slight muscle twitches on the face or hands; some patients may experience short-term discomfort, mild pain, Tinnitus, slight neurological disorders (such as hearing, cognition, etc.); some patients may even feel fainting. In one in ten thousand cases, brain magnetic stimulation has a chance to induce transient epilepsy while stimulating the brain. If the patient has implanted therapeutic equipment, such as pacemakers, defibrillators, etc., then doctors and medical staff will handle very carefully. The neurorehabilitation specialists and medical teams will work together to ensure the comfort of patients and strive to minimize the risks of treatment.
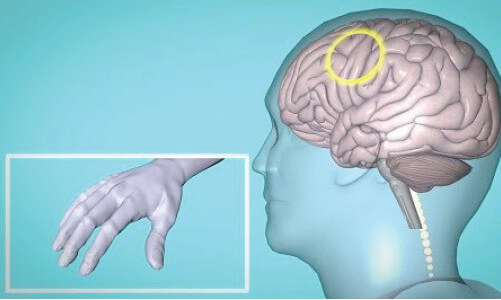
TMS stimulate certain brain area will trigger the right hand movement
The clinical use of brain magnetic stimulation therapy is used to help stroke patients recover their nerve function and the clinical application of brain magnetic stimulation therapy has been extended to other neurological diseases and mental health care, such as dementia in the elderly, anxiety disorders and depression. In addition, brain magnetic stimulation therapy is also used clinically to measure the activity and functionality of the human nervous system. Among them, the most widely used is to measure the motor cortex, one of the central nervous systems of the brain, the spine and the peripheral nervous systems of the limbs. The connection between these two systems and the nerve information transmission can be used to assess the damage caused by past and current neurological diseases in related brain structures and functions.
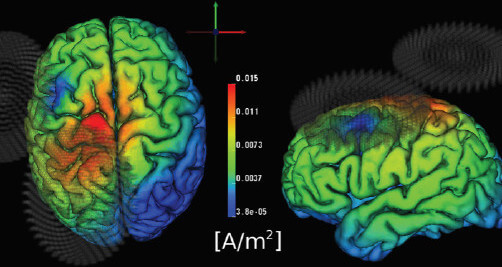
From MRI imaging, can see the brain is active under TMS ( color in red) whereas the other area is inactive without the TMS ( color in blue)
The course of treatment is about eight to ten weeks.
Once to twice a week
Each treatment lasts about 45-60 minutes.
During the procedure, patient does not use any anesthesia or sedative medication.
Brain Magnetic Stimulation TMS Treatment operated by Dr. Jennifer Myint and her trained medical staff.
Dr. Jennifer Myint is a specialist in Geriatric Medicine. Her main interest in Neurorehabilitation, neurostimulation therapy (including TMS and tDCS) , Dementia, Osteoporosis and Healthy Ageing.
Dr. Myint graduated from the Medical Faculty of the University of Hong Kong in 1992. Trained in the University of Hong Kong and subsequently in Australia with a Master degree in Geriatrics, Dr Myint started her career in Internal Medicine and Geriatric Medicine. In 2006, she was credentialed in the specialty of Rehabilitation Medicine and then worked in a 500 bed Rehabilitation Department as Chief of Services. Being an experienced and respected clinician, she also held positions in Non Governmental Organizations as well as in Professional Associations.



