Spinal Injection
- Home
- Non-Surgical Procedures
- Private: Chiropractic
- Services
- Spinal Injection
Spinal Injection
Epidural injection

An epidural spinal injection is a non-surgical treatment option that may provide either short- or long-term relief of radiating back pain.
When spinal nerves become irritated or inflamed due to a degenerative condition in the spine that is causing nerve compression, such as a herniated disc or spinal stenosis, the result may be severe acute or chronic back pain, as well as pain, numbness and muscle weakness that extends elsewhere into the body, such as the hips, buttocks or legs.
What Is An Epidural Spinal Injection?
What Is An Epidural Spinal Injection?
An epidural spinal injection involves delivering anti-inflammatory medication – typically a steroid combined with an anesthetic – directly into the area around the irritated spinal nerves that are causing the pain. This area is called the epidural space, and it surrounds the sheath-like protective membrane – ordura – that covers the spinal nerves and nerve roots. Steroids reduce nerve irritation by inhibiting production of the proteins that cause inflammation; the anesthetic blocks nerve conduction in the area where it’s applied, numbing the sensation of pain.
Facet Joint Injection
A facet joint injection, or facet block, is a non-surgical procedure in which a combination anesthetic/steroid is delivered directly into a facet joint in the spine that may be causing back or neck pain. The purpose of the anesthetic is to ease the pain; the steroid to relieve inflammation. The effects of the injection may be temporary or permanent, and the procedure also may be used as a diagnostic tool to determine whether the facet joint is the cause of the pain.
What Is A Facet Joint Injection?
What Is A Facet Joint Injection?
Facet joints connect the vertebrae, and provide for the stability and flexibility of the spine. There are two facet joints between each pair of vertebrae, one on each side. Facet joints link each vertebra to those directly above and below it, and allow the vertebral bodies to rotate with respect to each other. Cartilage in the joints allows for smooth movement where vertebral bones meet, and each is lined with a thin membrane called the synovium, which produces synovial fluid for lubrication.
If the facet joints and the tissues around them become inflamed and swollen, these irritated structures can compress one or more spinal nerve roots. The result may be localized and/or radiating pain and other symptoms, such as numbness and muscle weakness.
A facet joint injection, or facet block, is a non-surgical procedure in which a combination anesthetic/steroid is delivered directly into a facet joint in the spine that may be causing back or neck pain. The purpose of the anesthetic is to ease the pain; the steroid to relieve inflammation. The effects of the injection may be temporary or permanent, and the procedure also may be used as a diagnostic tool to determine whether the facet joint is the cause of the pain.
Transforaminal Injection
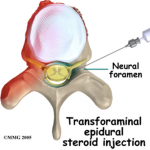
A transforaminal injection is an injection of long acting steroid into the opening at the side of the spine where a nerve roots exits. This opening is known as a foramen. There is a small sleeve of the epidural space that extends out over the nerve root for a short distance. This epidural root sleeve is just outside the spinal canal. Sometimes these injections are referred to as root sleeve blocks, root blocks or transforaminal epidural blocks.
Sacroiliac Injection
A sacroiliac injection is an injection of a steroid or other medication into a sacroiliac joint. The sacroiliac joints are located on either side or the sacrum or tailbone. They connect the tailbone to the pelvis.
Not recommend for spinal injection
Patient has neurological deficit, like foot drop or cauda equina syndrome from a lumbar herniated disc, surgery might be a better option to free the spinal cord or nerve to allow for better recovery
 Book an Appointment
Book an Appointment


